Understanding Black Mold
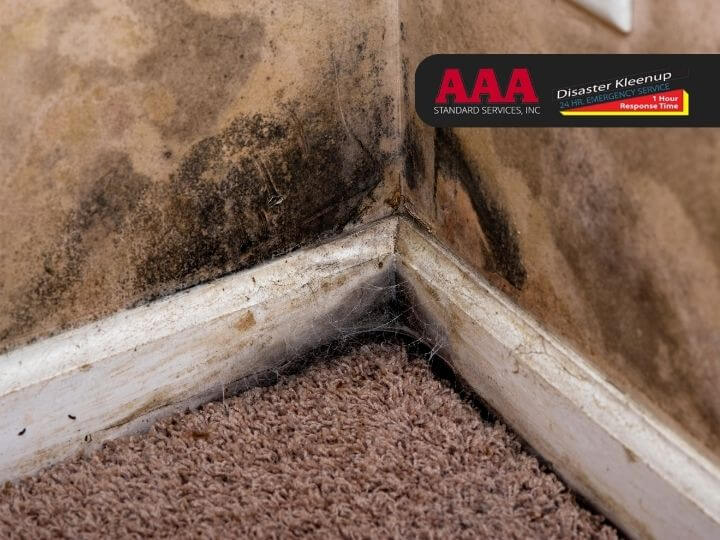
Stachybotrys chartarum, more commonly known as black mold, is a fungus that thrives in environments that are damp, dark, and humid. This mold, distinguishable by its black or dark green color, is often found in areas such as basements and bathrooms or in spaces that have suffered water damage. If you suspect the presence of this harmful mold in your living or workspace, it’s advisable to seek the expertise of AAA Standard Services, specialists in Professional Mold Inspection & Mold Testing.
When black mold grows, it releases spores into the air. These spores, when inhaled or touched, can have harmful effects on human health, especially for those with weakened or compromised immune systems. Exposure to black mold over a significant period or in large amounts can lead to a range of health issues, from minor allergies to severe conditions like respiratory problems or damage to internal organs. We will delve deeper into these health implications in the sections that follow.
The importance of understanding black mold extends beyond maintaining a clean household. It is crucial for protecting human health. In the upcoming sections, we will explore how exposure to black mold can potentially trigger autoimmune responses and mimic the symptoms of autoimmune disorders. We will also discuss strategies for preventing and managing black mold exposure to help maintain a healthy, mold-free environment.
Defining Black Mold
Black mold, often referred to as toxic mold, is a member of the Stachybotrys genus and the chartarum species. It is typically identified by its dark green or black color. The presence of black mold often indicates underlying issues such as moisture accumulation, leaks, or inadequate ventilation in a particular area.
What distinguishes black mold from other types of fungi is its production of mycotoxins, specifically of the trichothecene type. These compounds are released during the mold’s growth and reproduction phases. If the mold is disturbed, the spores carrying these mycotoxins can spread and contaminate the surrounding air and surfaces.
However, it’s crucial to note that not all black or dark-colored molds are Stachybotrys chartarum. Misidentification can lead to unnecessary alarm or neglect of other potentially harmful mold species. Accurate identification usually requires the expertise of professionals and laboratory testing. This complexity underscores the importance of maintaining a moisture-free and well-ventilated environment to prevent the growth of all types of mold.
Health Implications of Black Mold
Black mold, notorious for its production of mycotoxins, poses a significant threat to public health. The symptoms of short-term exposure often manifest in the respiratory system, leading to chronic coughing, sneezing, eye irritation, rashes, persistent fatigue, and recurring headaches.
The stakes rise with prolonged exposure, as the health effects become more severe. The continuous inhalation of black mold spores triggers an enduring inflammatory response, resulting in sinus infections, asthma attacks, allergic reactions, and chronic lung diseases.
The most concerning aspect of black mold exposure is its potential to compromise the immune system, especially in individuals already grappling with weakened immunity. Current research is exploring the link between black mold exposure and the exacerbation or onset of autoimmune disorders, a topic we will delve into in subsequent sections.
It’s important to underscore that no degree of black mold exposure is deemed ‘safe’. Any suspicion of its presence should be addressed immediately to mitigate potential health risks.
Autoimmune Disorders Explained
Autoimmune disorders represent a group of conditions where the immune system erroneously targets healthy cells, tissues, or organs. This misguided immune response leads to inflammation and damage, resulting in a wide range of symptoms that vary across different disorders.
The root cause of autoimmune disorders remains elusive, although genetics, environmental factors, and certain infections are thought to contribute to their onset. Examples of common autoimmune disorders include Rheumatoid Arthritis, Multiple Sclerosis, Lupus, Type 1 Diabetes, and Inflammatory Bowel Disease.
In these conditions, the immune response often involves the production of autoantibodies, proteins that attack the body’s own cells. This results in chronic inflammation and potential significant damage to the targeted cells or tissues. Immunosuppressive treatment is frequently used to manage these disorders, which can, unfortunately, render patients more prone to infections.
Common signs of an autoimmune condition include fatigue, fever, general discomfort, and difficulty concentrating. Interestingly, many of these symptoms are also associated with black mold exposure, sparking increased research interest in the potential link between the two.
Management of autoimmune disorders typically involves symptom monitoring, medication adherence, maintaining a healthy lifestyle, and regular medical check-ups. This underscores the necessity of identifying and mitigating potential environmental triggers, such as black mold, that could worsen these conditions. We will explore this connection further in the following sections.
Understanding Autoimmune Disorders
Imagine your body’s immune system as a dedicated sentinel, ceaselessly patrolling to detect and eliminate harmful intruders like viruses and bacteria. But what happens when this sentinel turns against its own? This is the perplexing reality of autoimmune disorders, where the immune system mistakenly attacks the body’s own healthy cells.
The spectrum of autoimmune disorders is broad and varied, with each disorder targeting different organs or tissues. For instance, Type 1 Diabetes is an autoimmune disorder where the immune system targets the pancreas. On the other hand, Lupus is a systemic disorder that can impact multiple organs and systems simultaneously.
The world of autoimmune disorders is a complex labyrinth within the medical field. Diagnosis can be challenging due to overlapping symptoms with other conditions. Interestingly, women are more prone to these disorders, and there are over 80 known types of autoimmune conditions.
The root cause of autoimmune disorders remains a mystery, but it’s believed to be a combination of genetic and environmental factors leading to an errant immune response. Adding to the complexity, it’s possible for an individual to have multiple autoimmune disorders concurrently.
Inflammation is a common thread in autoimmune disorders, resulting in symptoms like redness, heat, pain, and swelling. This inflammation can cause tissue damage, abnormal organ growth, and changes in organ function, leading to a variety of symptoms depending on the specific disorder and the body parts affected.
While there is no known cure for most autoimmune disorders, symptom management is possible. The primary aim is to suppress immune system activity, alleviate symptoms, control the autoimmune process, and maintain the body’s ability to combat disease. Living with an autoimmune disorder often requires managing flare-ups and reducing exposure to potential triggers, such as black mold, which we will delve into later.
Implications of Autoimmune Disorders on Health
The impact of autoimmune disorders on an individual’s health is profound. These conditions, characterized by the body’s immune system attacking its own cells, can affect any part of the body, leading to a myriad of health complications.
Chronic inflammation, a hallmark of these disorders, can cause damage to organs and tissues, disrupting normal body functions. This disruption manifests in various ways, including fatigue, body aches, cognitive impairment, and organ dysfunction, depending on the specific disorder.
The chronic nature of autoimmune disorders often leads to a diminished quality of life. The unpredictable cycle of flare-ups and remissions can significantly disrupt daily activities, leading to emotional distress and potential mental health conditions like anxiety and depression.
Treatment for autoimmune disorders can also pose challenges. Immunosuppressive treatments, which control an overactive immune response, can increase susceptibility to infections by weakening the body’s natural defenses.
Moreover, having one autoimmune disorder can increase the risk of developing another, further complicating health management. For example, individuals with Hashimoto’s thyroiditis have an increased risk of developing Celiac disease.
The health implications of autoimmune disorders extend beyond physical symptoms to include mental health, lifestyle changes, increased susceptibility to other illnesses, and lifelong management. This underscores the need for a comprehensive approach to managing these conditions, which may include avoiding potential triggers like black mold exposure.
Black Mold and Autoimmune Disorders: The Connection
The exploration of environmental triggers is a key component in the study and management of autoimmune disorders. One such trigger that has been gaining traction in research circles is black mold, scientifically known as Stachybotrys chartarum. This toxic mold is often found in damp and water-damaged buildings, releasing mycotoxins that can pose serious health risks when inhaled.
The potential link between black mold exposure and autoimmune disorders is an area of study that is still in its infancy. Preliminary research suggests that exposure to mold and its byproducts could potentially trigger or exacerbate autoimmune responses in individuals who are genetically predisposed. However, more extensive studies are needed to confirm these findings.
The importance of understanding this potential correlation cannot be overstated, particularly due to the overlap in symptoms between black mold exposure and autoimmune disorders. This overlap can make diagnosis and management of autoimmune disorders more challenging, but it also presents an opportunity to explore environmental factors as part of the treatment plan.
In the subsequent sections, we will delve deeper into the potential link between black mold exposure and autoimmune responses, as well as the similarities in symptoms between black mold exposure and autoimmune disorders.
Black Mold Exposure and Autoimmune Responses
The potential link between black mold exposure and autoimmune responses is a burgeoning area of research. The mycotoxins produced by black mold, or Stachybotrys chartarum, are harmful substances that could potentially influence immune responses.
From a scientific standpoint, black mold and its mycotoxins can trigger chronic inflammatory responses, akin to those observed in autoimmune disorders. These toxins can activate immune cells, leading to a state of sustained inflammation.
Such chronic inflammation could potentially worsen existing autoimmune conditions. The activated immune cells may not only attack the invading mold spores but could also begin damaging healthy body tissues, thereby intensifying autoimmune responses.
Furthermore, mycotoxins have been reported to disrupt the normal function of the immune system, pushing it towards hyperactivity, a common trait observed in autoimmune disorders. This disruption could potentially increase an individual’s susceptibility to developing autoimmune conditions.
It’s also important to note that black mold exposure may lead to an increase in the production of certain autoantibodies, proteins that mistakenly target and react with a person’s own tissues or organs. These autoantibodies are typically present in individuals with autoimmune disorders.
While these findings suggest a potential link between black mold exposure and autoimmune responses, it’s important to emphasize that more extensive studies are needed to fully understand the depth of this association and the mechanisms involved. Additionally, factors such as genetic susceptibility and other environmental triggers should be considered when discussing the role of mold exposure in the onset or progression of autoimmune diseases.
Similarities Between Black Mold Symptoms and Autoimmune Disorders
The intersection of black mold exposure and autoimmune disorders is not merely confined to potential mechanistic links. It extends to a significant overlap in their symptom profiles, which can often complicate diagnosis and management of an individual’s health.
The health implications of black mold exposure can range from persistent cough, eye irritation, and skin rashes to headaches, fatigue, and sinus congestion. In more severe cases, individuals may experience nausea, vomiting, and even bleeding in the nose and lungs.
Intriguingly, a number of these symptoms are also characteristic of various autoimmune disorders. For example, fatigue, headaches, and joint pain are frequently reported in conditions such as lupus and rheumatoid arthritis. Respiratory symptoms, including difficulty breathing, are often seen in autoimmune conditions like systemic sclerosis and Sjogren’s syndrome.
Furthermore, akin to autoimmune disorders, the impact of black mold exposure can be systemic, affecting multiple organs and systems in the body. Neurological symptoms such as cognitive dysfunction, memory loss, and mood changes, which are sometimes observed in individuals exposed to mold, are also associated with certain autoimmune disorders.
However, it’s crucial to understand that while the symptoms may appear similar, the underlying causes in black mold exposure and autoimmune disorders can be different. Hence, if an individual with an autoimmune disorder or autoimmune-like symptoms is exposed to black mold, healthcare providers should consider this exposure as a potential aggravating factor. This overlap in symptoms underscores the need for comprehensive medical evaluations and the consideration of environmental factors like black mold exposure in the diagnosis and management of autoimmune disorders.
Prevention and Management of Black Mold Exposure
Considering the potential health implications of black mold exposure, including the possible intensification of autoimmune conditions, it’s vital to arm ourselves with strategies to prevent and manage this exposure. A dual approach focusing on reducing the risk of black mold growth in our surroundings and implementing steps to manage health post-exposure can be highly effective.
Preventive strategies primarily revolve around controlling moisture and humidity levels, as black mold flourishes in damp environments. Post-exposure health management includes medical treatment, supportive care, and potentially, interventions to strengthen the immune system.
In subsequent sections, we will explore practical methods to prevent black mold exposure and effective ways to manage health after such incidents. It’s imperative to note that while these measures can help mitigate the black mold-autoimmune connection, they should be complemented by regular medical care and follow-ups, particularly for individuals with pre-existing autoimmune disorders.
Strategies to Prevent Black Mold Exposure
The key to preventing black mold exposure lies in creating an environment where it cannot thrive. This typically involves maintaining a dry, well-ventilated space. Here’s how you can achieve this:
Regulate Humidity: Aim to keep the indoor humidity below 50%. This can be accomplished with the use of dehumidifiers or air conditioners, as mold thrives in humid conditions.
Ensure Proper Ventilation: Good ventilation is crucial, especially in areas prone to moisture such as bathrooms, kitchens, and basements. Use exhaust fans and open windows whenever possible.
Address Leaks Immediately: Water leakage can create a perfect environment for mold growth. Therefore, it’s essential to repair leaks promptly and clean any water-damaged areas.
Quickly Dry Wet Areas: Wet areas can become a breeding ground for black mold. Whether it’s a spill on the carpet or water seepage in the basement, ensure these areas are dried quickly.
Inspect HVAC Systems: Regularly check and clean your heating, ventilation, and air conditioning (HVAC) systems to prevent them from becoming a source of mold distribution.
Opt for Mold-Resistant Products: If you’re renovating or building a new home, consider using mold-resistant products such as mold-resistant drywall or sheetrock, or mold inhibitors for paints.
Early intervention is crucial in dealing with mold problems, as they can quickly escalate. If you’re having difficulty controlling mold in your home, consider seeking professional help. By implementing these preventive strategies, you can significantly reduce the risk of black mold exposure and its potential health implications, including autoimmune disorders.
Managing Health After Black Mold Exposure
If you’ve been exposed to black mold, it’s crucial to manage your health promptly and effectively. Here are some strategies to consider:
Seek Medical Help: If you suspect mold exposure and are experiencing related symptoms, seek medical attention immediately. Providing your healthcare provider with detailed information about your exposure and symptoms can aid in accurate diagnosis and treatment.
Remediate Mold: If your home has been the site of exposure, immediate mold remediation is necessary. For large-scale infestations, professional mold remediation services may be required.
Undergo Treatment: Depending on your symptoms and their severity, your healthcare provider may recommend treatments such as antihistamines, nasal sprays or decongestants, and medications for joint pain and inflammation. If you have an autoimmune disorder, your treatment plan may need to be adjusted.
Practice Supportive Care: Rest, hydration, and a nutritious diet can aid in recovery. Avoid immune system suppressants like smoking and excessive alcohol. Regular exercise and meditative practices can also support immune health.
Monitor Symptoms: Regularly observe and document any changes in your health and promptly communicate them to your healthcare provider. This can help detect escalating issues or the onset of autoimmune-like symptoms.
In addition to these reactive measures, proactive steps to prevent further exposure are crucial. Remember, reactions to mold exposure can vary greatly among individuals, and those with pre-existing autoimmune disorders may experience more severe reactions. Therefore, personalized medical care and vigilant monitoring are vital after black mold exposure.